Why Lung Health Matters on World MS Day – And Every Day
Each year on May 30, the world unites to recognise World MS Day – a powerful movement that brings together the global Multiple Sclerosis (MS)
The respiratory tract is exposed daily to viral and bacterial pathogens, particulates and gaseous material with the constant threat of airway inflammation and infection (Bustamante-Marin & Ostrowski, 2017). The respiratory system uses several defence mechanisms against inhaled pathogens and particulates including cough clearance, anatomical barriers, aerodynamic changes and immune mechanisms, but the first line of defence of the lungs is the mucociliary clearance (MCC; Bustamante-Marin & Ostrowski, 2017).
The MCC is composed of airway surface layer (ASL) and hair-like structures called cilia. The ASL has two components—a layer of mucus that traps inhaled foreign particulates and pathogens and a low viscosity periciliary layer (PCL) that maintains moisture of the airway surfaces and promotes rhythmic ciliary beating for efficient mucus clearance (Bustamante-Marin & Ostrowski, 2017). In health, the synchronized rhythmic beating of cilia continuously transports the mucus with the foreign particulates and/or pathogen towards the pharynx where it is either swallowed or expectorated (Jing et al., 2017). Abnormal function of the cilia may lead to poor MCC, which is associated with various respiratory diseases, such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, sinusitis and chronic respiratory infections (Jing et al., 2017).
The respiratory system is divided into the upper respiratory tract or upper airway and the lower respiratory tract or lower airway. The upper airway includes the nose and nasal passages, paranasal sinuses, the oral cavity, the pharynx, and the portion of the larynx above the vocal cords, while the lower airway is further divided into conducting zone and respiratory zone. The conducting zone is formed by the portion of the larynx below the vocal cords, trachea, and within the lungs, the bronchi, bronchioles, and the respiratory zone are formed by the respiratory bronchioles, alveolar ducts, and alveoli. The percentage of airway ciliated cells increases from about 47% in the trachea to 73% in the small airway epithelium (respiratory bronchioles) (Tilley et al., 2015).
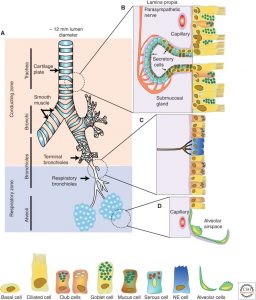
Cilia are present on epithelial cells lining the respiratory tract (Munkholm & Mortensen, 2014). Cilia are motile hair-like projections that are approximately 6µm long and 250 nm in diameter (Munkholm & Mortensen, 2014). The airway cilia beat in a coordinated fashion at low frequency (10-20 Hz) that results in metachronal waves (Bustamante-Marin & Ostrowski, 2017; Tilley et al., 2015). The waves travel across the epithelium, pushing the overlying mucus upward towards the pharynx to be swallowed (Bustamante-Marin & Ostrowski, 2017).
Aside from the ciliated cells, secretory cells are present in the airways that generate a deformable gel, known as mucus (Munkholm & Mortensen, 2014). In healthy airways, the mucus is lifted away from the cilia by the PCL, which is a low-viscosity periciliary liquid layer that prevents the mucus from adhering to the epithelial apical membrane, allowing the cilia to beat rapidly (Munkholm & Mortensen, 2014).
The respiratory system starts to form around the fourth week of gestation wherein the endoderm forms the epithelium and glands of the larynx, trachea, bronchi, and pulmonary lining epithelium (Bustamante-Marin & Ostrowski, 2017). After birth, the alveoli increase in number to reach the adult range of 300 million by 2 years of age (Bustamante-Marin & Ostrowski, 2017). The airway, on the other hand, does not increase in number, and the airway ciliated cells are incapable of self-renewal (Bustamante-Marin & Ostrowski, 2017; Tilley et al., 2015).
Smokers are at increased risk of respiratory diseases, such as respiratory tractinfections, and COPD. Several studies demonstrated that cigarette smoke causes inefficient MCC mechanism secondary to the following:

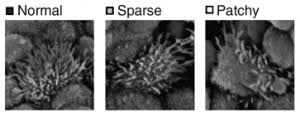
Decreased in numbers of ciliated cells, reduced cilia beat frequency and changes in intercellular coordination of the metachronal waves are associated with the smoking-related decrease in MCC efficiency (Leopold et al., 2009). The cilia height of smokers is found to be 10% shorter than nonsmokers (Leopold et al., 2009). The ASL height is constant, but the cilia height in smokers is reduced, decreasing the interaction between cilia and mucus on the forward stroke (Leopold et al., 2009). These mechanisms contribute to smoking-induced MCC dysfunction.
Several studies have shown a strong link between air pollutants and chronic respiratory diseases. Exposure to air pollutants impairs formation of new cilia. A recent study showed that air pollutants, such as vehicle exhaust and occupational dust, contain toxicological agonists that bind with aryl hydrocarbon receptor (AhR; Crotta et al., 2016). AhR functions as a transcription factor that is required for the formation of multiciliated cells and detoxification (Crotta et al., 2016). The presence of air pollutants in the airways triggers AhR to divert its focus away from forming new cilia to initiate a detoxification process (Crotta et al., 2016).
The diversion of AhR impairs the formation of new cilia, leading to a reduction of the number of cilia in the airway epithelium (Crotta et al., 2016). Lesser number of cilia leads to inefficient mucociliary clearance of pathogens and particles from the airways, resulting in respiratory diseases (Crotta et al., 2016). It is most likely that young infants are subjected to the effects of impaired AhR-mediated ciliogenesis, as this dysregulation predominantly occurs during the early phase of development (Crotta et al., 2016).
Primary Ciliary Dyskinesia (PCD) is an autosomal recessive disorder of motile cilia. Patients with PCD have ciliary motility but ineffective MCC (Tilley et al., 2015). PCD is associated with reduced cilia beat frequency, and dyskinetic cilia waveform, contributing to ineffective MCC (Tilley et al., 2015). The clinical manifestations of PCD include nasal congestion, chronic sinusitis, recurrent lower respiratory tract infection, bronchiectasis, neonatal respiratory disorders in newborns, chronic otitis media, transient hearing loss/speech delays, male infertility, and defects in organ laterality (50% of cases) (Tilley et al., 2015). Respiratory diseases in PCD are caused by defective MCC and worsen over time, secondary to repeated respiratory tract infections (Tilley et al., 2015).
Any deficiency in the mechanism of mucociliary clearance is associated with respiratory diseases, such as Asthma, COPD, cystic fibrosis, sinusitis, bronchiectasis and chronic respiratory tract infections. Use of therapeutic techniques that would help enhance MCC function is beneficial to patients with respiratory diseases, smokers, and individuals who are chronically exposed to air pollution.
AirPhysio® device is a handheld device that utilizes Oscillating positive expiratory pressure (OPEP) therapy, which effectively enhances MCC function and clears airway secretions in individuals with respiratory diseases, as well as in smokers and those with prolonged exposure to air pollution. OPEP reduces mucus viscoelasticity and makes mobilization of mucus up the airways easier to be either swallowed or coughed out (Myers, 2007). AirPhysio® reduces mucus accumulation in the airways, which may help improve lung function and health-related quality of life.

References
Bustamante-Marin, X. M. & Ostrowski, L. E. (2017). Cilia and mucociliary clearance. Cold Spring Harbor Perspective in Biology, 9(4), 1-17. doi:10.1101/cshperspect.a028241
Crotta, S., Ahlfors, H., Dingwell, K., & Smith, J. C. (2016). The aryl hydrocarbon receptor controls cyclin O to promote epithelial multiciliogenesis. Nature Communications, 1-11. doi:10.1038/ncomms12652
Jing, J. C., Chen, J. J., Chou, L., Wong, B. J. F., & Chen, Z. (2017). Visualization and detection of ciliary beating pattern and frequency in the upper airway using phase resolved Doppler optical coherence tomography. Scientific Reports, 7(8522), 1-11. doi:10.1038/s41598-017-08968-x
Leopold, P. L., O’Mahony, M. J., Lian, X. J., Tilley, A. E., Harvey, B., & Crystal, R. G. (2009). Smoking is associated with shortened airway cilia. PLoS ONE, 4(12), 1-11. doi:10.1371/journal.pone.0008157
Munkholm, M., & Mortensen, J. (2014). Mucociliary clearance: pathophysiological aspects. Clinical Physiology and Functional Imaging, 34, 171-177. doi:10.1111/cpf.12085
Myers, T. (2007). Positive expiratory pressure and oscillatory positive expiratory pressure therapies. Respiratory Care, 52(10), 1308-1327.
Tilley, A. E., Walters, M. S., Shaykhiev, R., & Crystal, R. G. (2015). Cilia dysfunction in lung disease. Annual Review of Physiology, 77, 379-406. doi:10.1146/annurev-physiol-021014-071931
Each year on May 30, the world unites to recognise World MS Day – a powerful movement that brings together the global Multiple Sclerosis (MS)
Asthma is more common than many people realise — affecting over 262 million individuals around the world. Yet despite how many lives it touches, asthma
In the pursuit of optimal respiratory health, understanding and implementing techniques like Chest Percussion can be a game-changer. This method, designed to enhance lung function
AirPhysio may be able to help by assisting with
✅Clearing the mucus clogging airways
✅Helps Promote Optimal Lung Capacity
✅Helps Promote Optimal Lung Hygiene
✅Helps treat Respiratory Conditions
✅May Reduce the chance of developing lung infections
✅Recommended by doctors, physical Therapists & Pulmonologists
✅Helps Make Breathing Easier
✅Sold in 106 countries globally


Do you suffer from Dry or Persistent Cough, Breathlessness, Respiratory or Severe Respiratory Conditions, or Shortness of Breath as you Get Older?

THIS PRODUCT MAY NOT BE RIGHT FOR YOU. READ THE WARNINGS BEFORE PURCHASE (Contraindications of Untreated pneumothorax; Tuberculosis; Oesophageal surgery; Right-sided heart failure; Middle ear pathology, such as ruptured tympanic membrane)
FOLLOW THE DIRECTIONS FOR USE
IF SYMPTOMS PERSIST, TALK TO YOUR HEALTH PROFESSIONAL

Gallery
AirPhysio is an Oscillating Positive Expiratory Pressure (OPEP) device that is used for mucus clearance and lung expansion to help in the treatment of respiratory conditions. The use of the AirPhysio device helps to facilitate secretion mobilization and maximize lung volume for cleaner healthier lungs.
© AirPhysio 2022 – All Rights Reserved
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |